Patient Information
At Rural Health Group, we believe every patient is entitled to quality and affordable Health Care. We accept most private insurances including BCBS, Medicare and Medicaid. We require your insurance co-payments, deductible at the time of visit. We accept cash, check and credit card. If you have questions about your insurance or coverage, call our office and ask to speak to a member of the Billing Department. If you have trouble paying for your health care due to your financial situation, please read the section below about our Sliding Fee Program and contact your provider’s office for questions.
New Patients
If you are a new patient, listed below is our new patient packet information. By completing this information prior to your appointment, you can significantly reduce the amount of time you spend in the waiting room. Click on the link(s) below to download the New Patient Packet. Print it out, fill it out, and bring it with you. This information will be reviewed with you annually.
MEDICAL and DENTAL – New Patient Packet
- Patient Agreement
- Acuerdo del paciente
- Notice of Privacy Practices
- Notificación de Prácticas de Privacidad
- Sliding Fee Application
- Verificación de Ingresos (Para Tarifa de Descuento)
- Income Assessment
- Evaluación de ingresos
Paying for Your Visit
Payment options include:
Cash, Checks, Visa, MasterCard, Discover and American Express.
Care Credit (Dental and Women’s Health).
Payment(s) can be made electronically via the Patient Portal.
Rural Health Group is not a “free clinic” – however, our services are available at a deeply reduced fee to those who qualify based upon household size and income. If you qualify for the Sliding Fee Discount Program, we will not deny service due to inability to pay. Inability to pay is explicitly defined as those patients with annual household income of 200% and below the federal poverty level.
Good Faith Estimate (GFE) for Health Care Items and Services Under the No Surprises Act
You have the right to receive a “Good Faith Estimate” explaining how much your health care will cost, under the law, health care providers need to give patients who don’t have insurance or who are not using insurance an estimate of the bill for health care items and services.
- You have the right to receive a Good Faith Estimate for the total expected cost of any non-emergency items or services that are scheduled at least 3 days in advance. This includes costs of your visit with the provider and related costs like lab tests, prescription drugs, equipment, etc. that are associated with the visit.
- You can also ask your health care provider for a Good Faith Estimate before you schedule an item or service.
- You should receive a Good Faith Estimate in writing at least 1 business day before your qualifying medical service or item or within 3 business days of your request for an estimate of costs prior to scheduling an item or service.
- If you receive a bill that is at least $400 more that your Good Faith Estimate, you can dispute the bill. To start the dispute process, contact Rural Health Group Billing Director at 252-536-5844.
- Make sure to save a copy or picture of your Good Faith Estimate.
For questions or more information about your right to a Good Faith Estimate, call the RHG Billing Department or visit www.cms.gov/nosurprises/
Sliding Fee Program
Rural Health Group believes that access to health care is a fundamental right that should not be limited by an individual’s ability to pay. Rural Health Group receives modest federal support to provide care to people with limited financial means. It is the intent and purpose of Rural Health Group Inc.’s sliding fee program to guarantee that all patients have access to quality medical care, regardless of their ability to pay for such services. Individuals with annual household income greater than 200% of the federal poverty level are considered ABLE to pay, and Rural Health Group may deny services for individuals earning more than 200% of federal poverty for non-payment. Rural Health Group’s sliding fee program is the payer of LAST resort. As such, if a patient qualifies for full Medicaid the patient is ineligible for the Sliding Fee Program. Having insurance does not disqualify you from the sliding fee program; it is determined based on household size and income.
- Medical / Dental: 2024 Sliding Fee Guidelines
- Médico / Dental: 2024 Pautas de la tarifa móvil
- Sliding Fee Application
- Verificación de Ingresos (Para Tarifa de Descuento)
Eligibility
Patients will qualify for sliding fee discounts based on household size and income. Eligibility is extended to all patients, regardless of other medical coverage, with the exception of NC Medicaid. Patients with limited Medicaid coverage may be screened for sliding fee. Patients can be insured and still qualify for sliding fee. Oftentimes we have patients with limited financial means who have Medicare or private insurance, but these individuals face barriers to paying co-payments, co-insurance, etc. Any insured patient who is having a hard time paying for medical services will be screened for sliding fee based on eligibility requirements of household size and income.
Release of Information
A Release of Information form is required by HIPAA laws whenever private health information (PHI) is used or disclosed for a purpose not specifically required or permitted by the Privacy Rule.
RHG Authorization for Release of Medical Information Form
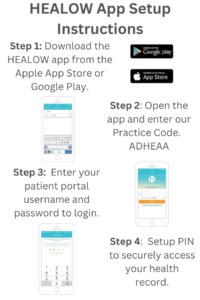
Patient Portal
Patients can utilize our patient portal to send messages to their care team, view lab results, view visit summaries, view medication list and request refills, view billing statements, and join televisits. The portal can be accessed via the patient portal website, or by downloading one of our HEALOW apps.
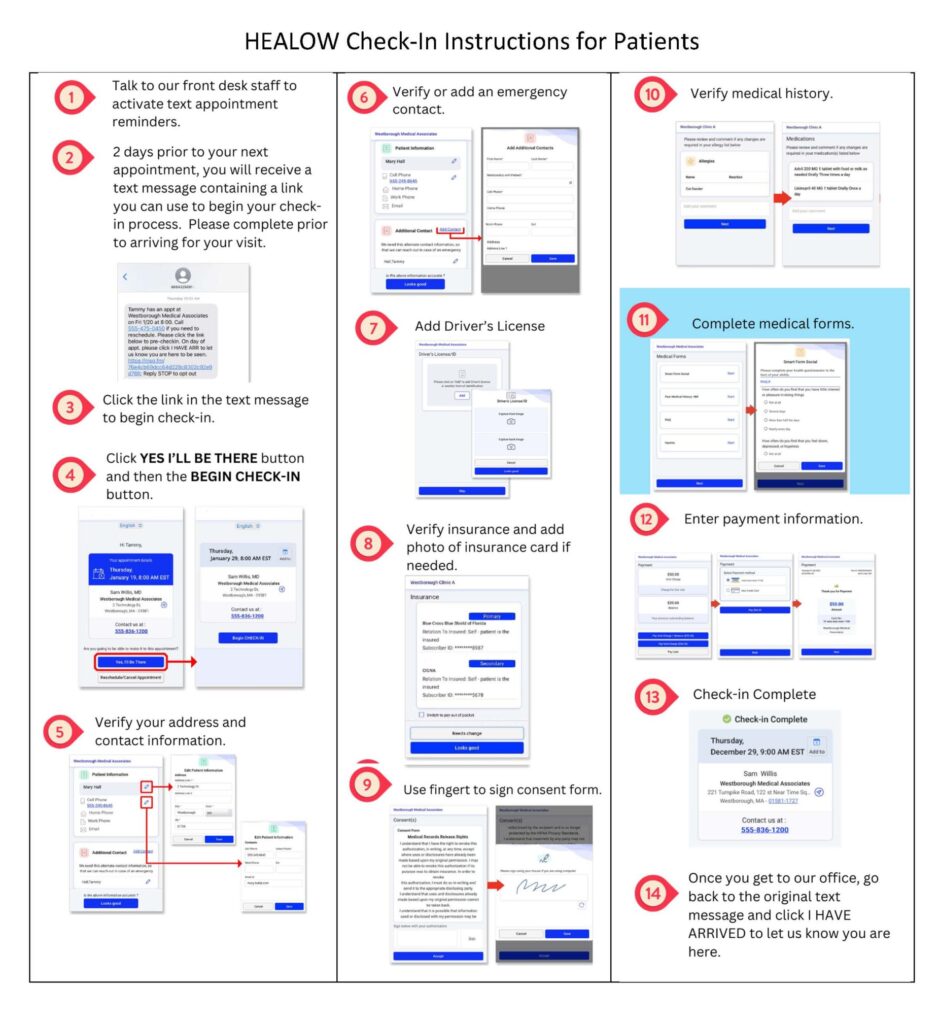
HEALOW Check-In
We have implemented a new patient check-in product called HEALOW Check-in. HEALOW check-in is a contactless solution that lets patients complete and sign forms, update demographics and insurance information, and check in for their appointments on a smartphone or computer from anywhere.